
8.20.20
A 25 year old Pamlico County resident was hospitalized for two weeks with COVID-19. We thank him for his willingness to talk about his experience with a member of the COVID-19 Community Task Force. His message is: “This no joke, man. This is real.” Read more about his experience below.
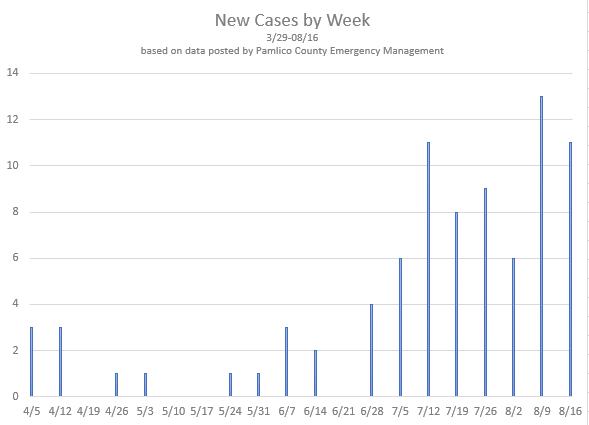
Local Statistics
On August 19, Pamlico County Health Officials announced a second death in the County attributed to COVID-19. As of 8/19, the County has reported a total of 85 cases; 8 cases are still active, 75 have recovered, and 2 have resulted in death. Nearby, Craven County has reported a total of 798 cases and 22 deaths; Carteret County has reported 392 cases and 5 deaths.
These graphs reflect Pamlico County COVID-19 case data as of August 16. 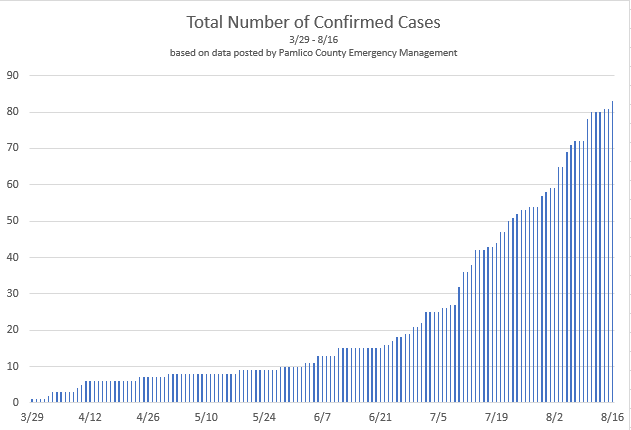
AB* is a 25 year old Pamlico County resident diagnosed with COVID-19 in late June and was hospitalized for 2 weeks. He agreed to share his story with a member of the COVID-19 Community Task Force to let people know this is a very real disease. Prior to his diagnosis, he thought COVID-19 was a hoax. He did not wear a mask, except at work where it is a requirement. And he did not pay particular attention to social distancing and hand washing.
He was not feeling well for several days, but did not think much about it. He thought maybe he was dehydrated because of the heat and continued to do his usual activities. But he continued to feel worse – feeling “very low” and “dragging”. After 3 days he went to Urgent Care where he was noted to have a temperature of 101.5. He was not aware he had a fever at that time. Urgent Care sent him to the hospital emergency room.
By the time he arrived at the emergency room he was having shaking chills and feeling even worse. He was admitted with suspected COVID-19, which was confirmed on testing. His x-ray showed pneumonia. He required oxygen during his hospital stay to keep his oxygen level in the normal range, but he did not need admission to the ICU. He reports one incident during the night when his oxygen mask came off and his oxygen saturation dropped into the 40’s. He does not entirely recall what happened, but the staff told him they were not sure he was going to make it at that point. Based on WHO criteria (pneumonia with one of the following – respiratory rate > 30, severe respiratory distress or oxygen saturation < 93% on room air), his symptoms would have been classified as severe.
He does not know what medications he received while in the hospital.
As far as AB knew, he was in good health; however, while he was hospitalized he was diagnosed with diabetes and sleep apnea. Because he did not know he had diabetes, his blood sugars were not in control. The uncontrolled diabetes probably contributed to his body’s response to the virus.
Finally, at the end of two weeks, his fever had resolved and his oxygen levels were in the normal range on room air, so he was discharged. After another two weeks at home, he has still not returned to work. He reports that he gets short of breath easily and he feels like his legs will give out if he tries to climb stairs.
Contact tracing was carried out. The person he had been staying with also tested positive. In hindsight, AB most likely contracted the virus from his friend. His friend was also not following recommended guidelines to decrease the risk of contracting or spreading the virus and had recently travelled to several places, including Myrtle Beach. Prior to the onset of AB’s symptoms, his friend had a few days where he was not feeling well, but symptoms were mild and were ignored.
His employer, coworkers, family and friends were affected too. The unit where he works was shut down until his coworkers were known to be negative. His other contacts, including his Mother and other friends, also had to quarantine until test results were available. None of them tested positive, besides his roommate.
Important points to learn from this story:
- Follow the 3 W’s. Wash your hands, keep your distance from others and wear a mask.
- Know what mitigation strategies your household members, as well as friends and family you associate with, are doing. Being in close contact for a minimum of 10 -15 minutes
with someone who is infected increases your risk of getting infected, especially if that person is not wearing a mask. If you are living with others or getting together with others who are not being careful about what they are doing or where they are going, there is a higher risk they may be infected. Choose your associates wisely!
- Assume everyone is infected regardless of their age. Infected individuals are shedding virus and are thus contagious to others starting about two days before the onset of symptoms, and remain contagious when they become symptomatic. AB continued to go about his normal activities for three days before seeking medical care, so there was a five day period he would have been contagious and out in the community.
- Pay attention to how you are feeling. If you are not feeling as well as you normally do, you must consider the possibility of COVID-19. As a minimum, stay at home and monitor your symptoms. Discuss how you are feeling with your health care provider or you can check your symptoms online to get guidance for what you should do: https://ncdhhs-covid19-dtra.powerappsportals.us/en-US/. AB very quickly developed severe symptoms.
- Be aware of what happens if you are identified as a contact of an infected individual. Contacts will be instructed to self-quarantine, which means you are not to leave your home, for two weeks or until you have tested negative. The work place of the infected individual will need to be closed until other employees are known to be negative.
AB’s message to everyone is “This no joke, man. This is real.” He and his family members and friends are now wearing masks and keeping their distance from others, as well as limiting their activities that expose them to groups of people.
*AB is not the actual initials of the patient, and the name is withheld for the patient’s privacy
Download a PDF of this Article